Many organisations supporting people in health and social care settings have clear policies and procedures, as well as training around the use of restrictive practices. The RRN training standards and guidelines have helped to balance the focus on ‘managing behaviours of concern’ being purely about how staff react at the time the behaviour occurs, to include discussions around more proactive approaches. Despite this we know that inappropriate and overuse of all types of restrictive practices can still be an issue within certain services or settings. In the case of some restrictive practices organisations, are not overseeing the regularity of their use due the difficulty in collecting this information.
What do we mean by Restrictive Practices?
When we talk about restrictive practices, we are not just referring to physical interventions. There are many types of restrictions that are often put into place and sometimes not even considered a restriction.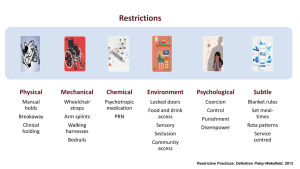
Restrictive interventions, such as physical restraint, seclusion, and the use of chemical or mechanical restraints, as well as more subtle restrictions that can be in place due to service structures, staffing and rotas, are employed often in place in health and social care settings, with the former used to manage situations where an individual’s behaviour presents a risk to themselves or others. While these interventions are sometimes necessary to ensure safety, they carry significant ethical, psychological, and professional implications. Among the most critical factors influencing the appropriateness and outcomes of restrictive interventions is the attitude of staff members responsible for administering them.
1. Impact on the Outcomes for People Supported
The attitudes of staff toward restrictive interventions can directly impact the well-being of people supported. When staff view these interventions sometimes necessary, where there is a legal implication of their use, as a last resort and approach their use with empathy and a strong ethical framework, they are more likely to apply the least restrictive option and monitor the individual closely. Positive staff attitudes help minimise harm, reduce the duration of the use of these practices, and prevent potential physical or psychological trauma to the person.
On the other hand, negative or indifferent attitudes toward restrictive practices can lead to overuse or unnecessary escalation. Staff members who lack empathy or proper training may resort to restrictive practices quickly, and appropriately without considering alternative de-escalation techniques, resulting in adverse effects, including increased distress, injury, or long-term psychological harm. Furthermore, people are more likely to experience feelings of humiliation, fear, or anger when they perceive staff as uncaring, excessively controlling or punitive in their approach.
2. Influence on the Organisational Culture
Staff attitudes also shape the overall culture within a healthcare or social care organisation. When an organisation prioritises person-centered care, training in de-escalation, and alternatives to restrictive practices, staff are more likely to adopt an approach that values dignity and respect. In such environments, restrictive practices are only used when necessary, with consideration of the law and the person’s best interests. High use is seen as a failure of other approaches rather than a default solution. Oversight and monitoring here is essential; so that feedback to the team about how the progress they are making in reducing their use of restrictive practices or maintaining a low level. Using a system like PBS Champion software makes this quick and easy to do. This fosters a culture of continuous improvement, where staff members seek to learn from behavioural incidents and explore less invasive methods to manage the risks associated with behaviours of concern.
Conversely, a permissive attitude toward restrictive practices, including a lack of knowledge about the frequency of these practices within an organisation, can normalise their use, leading to an over-reliance on these methods. Staff may become desensitised to the impact these interventions have on individuals, and the culture may discourage innovation or alternative approaches. In extreme cases, a negative organisational culture can contribute to a vicious cycle of escalating behaviour from people supported and more frequent use of restraint or seclusion, damaging the relationship between people supported and their teams. This then leads to increased risks for all.
3. Legal and Ethical Considerations
Restrictive interventions carry significant legal and ethical responsibilities. Most countries and healthcare systems have clear guidelines and regulations outlining when and how these interventions should be used. Staff members with positive attitudes toward these ethical principles are more likely to follow protocols, document incidents accurately, and ensure that the rights of individuals are respected.
Moreover, staff members who view restrictive interventions through an ethical lens are more likely to engage in reflective practice, seek supervision, and advocate for the rights of individuals in their care. This proactive stance helps to reduce the risk of abuse or misuse of interventions and aligns with legal standards that aim to protect vulnerable individuals.
4. Staff Well-being and Professional Satisfaction
The attitudes of staff toward restrictive practices also impact their well-being. Using physical or chemical restraints can be physically and emotionally taxing for staff members, especially when they feel unprepared, unsupported, or conflicted about their role in administering these interventions. Staff who hold negative or ambivalent views toward restrictive interventions may experience moral distress, guilt, or burnout, particularly if they feel they have no choice but to use them frequently.
On the other hand, staff who feel confident in their ability to manage challenging situations without relying on restrictive practices and are clear about the legal standing on any of the practices in use in their services interventions are more likely to experience greater job satisfaction. Positive attitudes toward de-escalation techniques, conflict resolution, and person-centered care can empower staff, reduce workplace stress, and promote a more supportive and collaborative work environment. This ultimately benefits both staff and people supported, as a motivated, well-trained, and ethically grounded workforce is better equipped to provide high-quality care.
5. Training and Professional Development
Staff attitudes toward restrictive interventions are often shaped by their training and professional development opportunities. Organisations that invest in comprehensive training programs, including those that have a high focus on proactive strategies such as PBS Training, as well as de-escalation techniques, trauma-informed care are more likely to cultivate positive staff attitudes. In contrast, a lack of training can lead to fear, uncertainty, or frustration among staff members when faced with behaviours of concern.
How to Gain Understanding about Staff Attitudes
Managers and services leads are best placed to understand the attitudes of their teams. However, it’s important that this is done with a degree of sensitivity to avoid staff taking a defensive stance or feeling picked out. Below are a few ideas
- Talk through both the pros and cons of specific practices used with your services in a team meeting. This enables teams to think about both the down sides and risks as well as the potential benefits for the person.
- Review the legality of each practice in place is important so that teams understand their has to be a legal justification for any practices in place.
- Looking at the current use of each restrictive practice and talk through with the team potential alternative practices that are not restrictive. Using a system like PBS Champion software which records all restrictive practices used during any behavioural incident will help to collate this information and allow that reflection.
Conclusion
The attitudes of staff toward restrictive interventions play a crucial role in shaping the care and support provided to people in healthcare and social care settings. Positive attitudes grounded in empathy, ethics, and a commitment to least restrictive practices can significantly improve outcomes for people, reduce harm, and enhance the support environment. Conversely, negative or indifferent attitudes can lead to overuse, people supported distress, and a breakdown in trust between staff and people receiving support. By ensuring that they understand staff attitudes and the number and types of restrictive practices in their services, organisations can ensure that these restrictive practices are used appropriately and ethically, with the best interests of both staff and people supported in mind. PBS Champion software provides a system for collating and reviewing all types of restrctive interventions, click on the links below to find out more.
Find out more https://redstonepbs.co.uk/pbs-champion/
Link to free walkthrough https://courses.onlinepbstraining.co.uk/courses/pbs-champion
View our brochure https://redstonepbs.co.uk/wp-content/uploads/2023/10/17082023-PBS-Champion-Brochure-Sept2023.pdf
Book a live demo email pbschampion@redstonepbs.co.uk
PBS Champion
PBS Champion provides a way to analyse the detail of incidents and ABC’s with the aim of gathering information about function. However, it also provides the ability to analyse behavioural incidents and any restrictive interventions at individual, service and organisational levels. This provides a very quick and easy way to report reductions in behavioural incidents as a result supports being put into place, as well as the reduction of any restrictive interventions used, evidencing the effects of RRN standards across an organisation.
If you’re interested in finding out more or to arrange a free demo for PBS Champion contact info@redstonepbs.co.uk
Author
Kate Strutt – Director of Redstone PBS and Clinical Psychologist.
Kate has over 20 years’ experience of working with adults and children with intellectual disabilities and those who are autistic, both within statutory services and the independent sector. Kate is registered with the Health and Care Professions Council. Bsc Psychology, D.Clin Psyc, MSc Applied Behaviour Analysis.